Describing an innovative framework to support school-aged childhood immunisations.
A framework to support healthcare support workers (HCSWs) to deliver school-aged childhood immunisations was developed in the school nursing service within the Rochdale Care Organisation, part of the Northern Care Alliance NHS Foundation Trust. This article aims to share the framework and the underpinning development work that led to this innovative change in practice, so that others may adapt and apply this to their own setting.
The HCSWs from the Rochdale school nursing service, who were redeployed to support the Covid-19 vaccination programme, thoroughly enjoyed the role they played in administering immunisations. After returning to the school nursing service, they expressed a desire to retain and further develop the knowledge and skills that they had gained during this experience.
The school nursing service is pivotal in the delivery of the school-aged childhood immunisation programme. Historically school-aged immunisations have been administered by school nurses (SNs) rather than HCSWs. School nursing is a profession where the professional demands have increased, but the numbers of practitioners within the profession have not.
Immunisation sessions depend on schools providing appropriate facilities and organising the flow of young people to the session. The sessions are reliant on the school timetable, therefore at times there can be a build-up and consequently a backlog of young people waiting for immunisation. It is imperative that young people are immunised as quickly as possible to prevent them from being out of class for longer than necessary and to ensure minimal disruption to the school day.
The project management team – which comprised the service manager for school nursing, the quality matron for children’s community services and the lead pharmacist for community services – explored the feasibility of enabling HCSWs to administer immunisations to young people. This was seen as a service development opportunity to enhance the HCSW role, making it more attractive, potentially improving retention and attracting new recruits to the service. Additionally, within a framework, extension of the HCSW role is a safe and pragmatic way of increasing the available workforce to administer immunisations as part of the school-aged childhood immunisation programme.
The risks and benefits associated with enabling HCSWs to administer elements of the school-aged immunisation programme was carefully considered. In principle the project management team believed that with a robust framework in place HCSWs could be enabled to administer school-aged immunisations. This development was supported by both the director of nursing and the director of pharmacy; NHS England has expressed its backing for this unique initiative during immunisation development meetings.
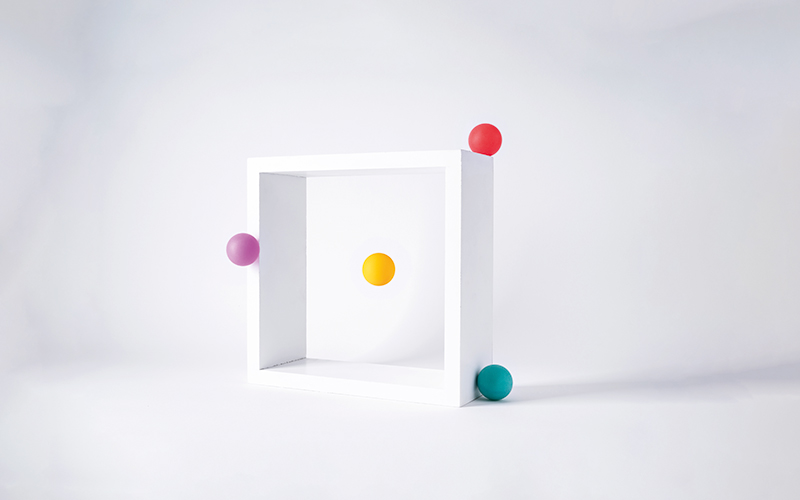
The framework that was developed to support the project includes the following:
- Independent prescribers, otherwise known as V300 non-medical prescribers (NMPs), with expertise of the childhood immunisation programme, assess the young person’s suitability to be immunised by a HCSW based on responses to health questions included as part of the informed vaccination consent form.
- NMPs write a patient-specific direction (PSD) on an individual basis for the young person deemed suitable to be immunised by a HCSW.
- A pre-immunisation checklist (see Pre-immunisation checklist below) was designed for the HCSW to complete with the young person prior to administering the immunisation.
- Pre-immunisation checklist completed by the HCSW with young person prior to administering the immunisation
- If requirements are not met, the HCSW refers the young person to the immunisation lead nurse responsible for the coordination of the immunisation session.
What is a PSD?
A patient-specific direction (PSD) is the traditional written instruction, signed by a prescriber for medicines to be supplied and/or administered to a named individual after the prescriber has assessed that individual on a one-to-one basis (Specialist Pharmacy Service, 2023).
Training and competency development
The V300 prescribers involved in the initiative were provided with bespoke training on the writing of a PSD for the school-aged childhood immunisations. This was delivered by the lead pharmacist for community services, who also delivered training to the HCSWs on interpretation and utilisation of a PSD.
The Northern Care Alliance clinical skills team developed and delivered training on injection technique for the HCSWs. Additionally, the framework outlines the necessity for HCSWs to remain compliant with basic life support (BLS), paediatric basic life support (PBLS) and anaphylaxis mandatory training. It should be noted that HCSWs are expected to receive anaphylaxis training to enable them to identify signs and symptoms so that they are able to alert the registered staff and provide basic first aid. HCSWs are not permitted to administer adrenaline.
A competency assessment framework was developed to ensure that the HCSWs were competent and confident to administer school-based immunisations. Furthermore, the function of administering immunisations was added to the HCSW job description to ensure coverage under the Clinical Negligence Scheme for Trusts (CNST).
Additional opportunities and resources
Some of the HCSWs are based in Healthy Child Programme (HCP) teams rather than the immunisation team. The HCP teams are linked to schools. The service development included allocating the HCSWs to the immunisation sessions being delivered in the schools to which they are linked – not only developing their clinical skills, but also widening networking opportunities.
This service development required an increase in the number of V300 non-medical prescribers within the school nursing service. It has therefore created an opportunity for the school nurses to access the V300 course. Overall, an additional four SNs have been trained, with a further two scheduled to complete the course by April 2023.
As an interim measure, to initially support the service development, V300 prescribers from the health visiting service assisted in completion of the PSDs, widening their scope of practice and further harnessing opportunities for collaborative working across the 0 to 19 years service.
All five Band 3 HCSWs working within the school nursing service have received the essential training, been assessed as competent and are administering school-aged immunisations.
Pre-immunisation checklist
- Consent in place
- PSD in place
- Child feels well
- No allergies, medical conditions or medication other than that already disclosed
- No injections in the last month
- Not pregnant
Learning
The service development has been operational since November 2021. There were a few initial teething problems that needed to be addressed – the most significant being the wording of the pre-immunisation checklist, which was limiting the number of children that the HCSWs could immunise. Initially the pre-immunisation checklist asked:
- Do you have any allergies?
- Do you see any health professional regularly for any health problems?
- Do you take any regular tablets or medicines?
The HCSWs interpreted this to mean that if the young people answered yes to any of these questions, they could not administer the immunisation, even though anything disclosed on the consent form had already been reviewed by the V300. The question was changed to the following statement:
- Have no allergies, medical conditions or taking medication other than that disclosed on the consent form.
This resolved the presenting issue.
Evaluation
Initial feedback from the school nursing team leader indicated that the HCSWs embraced the role extension and worked conscientiously through their competency framework. In doing this, they provided observations and feedback to the registered nurses, who reflected on their own practice. This allowed the service to critically reflect on immunisation session delivery.
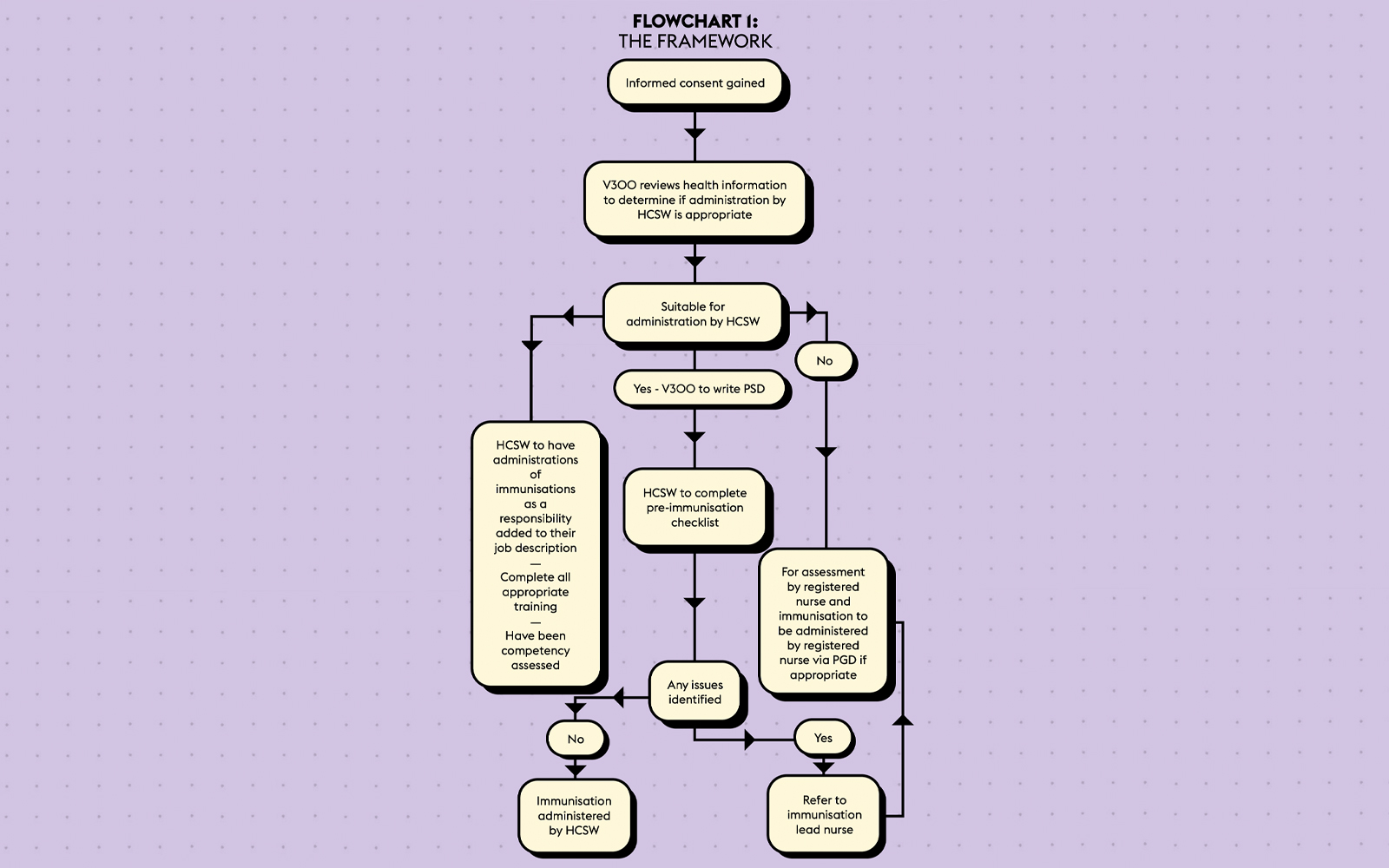
A formal evaluation has taken place in the form of two focus groups, facilitated by a lead nurse independent of the service. Areas discussed within the focus groups are outlined in Table 1, below.
Participants of the first focus group included two HCSWs (trained to immunise); the second included a school nurse from the immunisation team and a school nurse from the HCP team. The focus groups took place face to face and were recorded and transcribed using the Microsoft Teams record/transcription function. Unfortunately, the transcriptions from the Microsoft Teams recordings were inaccurate due to the overlap of voices during the focus group. Transcription was therefore undertaken manually, and subsequently transcriptions were reviewed and coded in line with thematic analysis. Analysis was undertaken by the main author RB and subsequently checked again by co-author NS.
Themes emerging from the data included:
1. Increased variety of role and job satisfaction
Participants described how the development of the skill to immunise has been a great opportunity that has brought variety to their role; they also report that it has greatly increased their job satisfaction and confidence. HCSW A said: ‘Oh, I love it. I really, really do enjoy doing it. It’s the variety I suppose.
‘You know, I’ve worked in the NHS 31 years, so I’ve done it a long time and you get in a bit of a rut … this has been a nice change, learning a new skill.’
2. Robust training and competency development
The conversations outline that while some HCSWs may have had an element of apprehension about their involvement in administering immunisations to young people, they felt that the training they received was robust and they were not rushed to develop the competencies that equipped them for the role. In fact, the HCSWs highlighted that they felt that the competency development was a little slow and could have been completed more quickly, although they do recognise that the management team was trying to protect them by preventing them from feeling rushed.
3. Positive impact on teamworking
Focus group participants believed that the service development has had a positive impact on team-working. The HCSWs feel that they are better able to support the nurses in the immunisation sessions and the nurses think that the HCSWs being able to immunise makes a huge difference to the running of the immunisation sessions. There is clear evidence of a mutual respect of each other’s roles within the transcriptions. HSCW B said: ‘This development has been really big – it’s helped me feel like part of more teams.’
4. Increased efficiency of the service
The service development has enabled the service to increase immunisation capacity and direct appropriate resource, resulting in the sessions running more smoothly. The more efficiently run sessions have been shorter or have reduced the need for the school nursing team to return to a school to deliver a further immunisation session. However, both groups do highlight the original issue with the wording of the pre-immunisation checklist, which impacted on the flow of young people through the session at the beginning of the project.
The positive impact of the quick and efficient flow of children through an immunisation session is highlighted in the focus groups, especially for those children who may be feeling stressed or emotional at the thought of having the immunisation. The faster flow of young people means that they are not as anxious because their waiting time is reduced. Additionally, the school staff are happier that the sessions are streamlined, and the young people are spending less time out of the classroom. SN A said: ‘I felt like the sessions that I’ve been to … ran really well, like that it made a difference having the healthcare support workers there.’
The feedback from the focus groups has highlighted a further learning point to the project management team. Covid-19 has created a backlog of outstanding school-aged immunisations that necessitated deployment of HCSWs to immunisation sessions other than those delivered in schools that they are linked to. This has resulted in some of the HCSWs feeling that they may have missed updates in their HCP team. This will be considered moving forward.
All staff involved in the focus groups expressed a strong desire for the initiative to continue.
Summary and next steps
The initiative has achieved the original aim of optimising the job satisfaction of HCSWs and improving the flow of young people through immunisation sessions, with all the consequential impacts described in the paper. There has been learning throughout the journey and indeed there may be more to come as the service development becomes embedded into practice.
The framework was a safe and effective means of implementing a change to service provision. This has led to several improvements, including improved flow and an ability to increase the number of young people vaccinated in any given session. Additionally, both HCSWs and SNs involved in the initiative report feeling more valued and having increased job satisfaction, underpinned by increased knowledge and experience related to delivery of the immunisation program.
‘I felt like the sessions that I’ve been to ran really well, like it made a difference having the healthcare support workers there’
It is understood that enabling HCSWs to administer school-aged immunisations is a novel approach and we are not aware of this innovation being implemented elsewhere. The framework that has been put in place in Rochdale is completely replicable, albeit with potential adaptations to meet local contextual factors.
Richelle Buckley is quality matron, Rochdale Community Service; Nicola Sharp is service manager school nursing; Robert Hallworth is lead pharmacist, community services, all at Northern Care Alliance NHS Foundation Trust.
Acknowledgements:
Charlotte Towell, lead nurse community assessment accreditation, Northern Care Alliance NHS Foundation Trust; and Heather Iles-Smith, professor of nursing, University of Salford.
References:
Royal College of Nursing. (2022) Non-medical prescribers. See: rcn.org.uk/get-help/rcn-advice/non-medical-prescribers (accessed 3 February 2023).
Specialist Pharmacy Service. (2023) Patient specific directions. See: sps.nhs.uk/articles/questions-about-patient-specific-directions-psd (accessed 15 February 2023).
UK Health Security Agency. (2013) Immunisation by nurses and other health professionals: the green book, chapter 5. See: gov.uk/government/publications/immunisation-by-nurses-and-other-health-professionals-the-green-book-chapter-5 (accessed 3 February 2023).
Image credit | Getty